What Is ALS?
This neurodegenerative disease has been getting some much-needed research focus

AARP (SOURCE: ALAMY STOCK PHOTO (2), GETTY IMAGES)
Remember the Ice Bucket Challenge? It’s been 10 years since social media feeds were saturated with videos of people willingly having large buckets of ice water dumped over their heads to raise money for ALS research.
More than 17 million people took the challenge in 2014 to speed research on amyotrophic lateral sclerosis, or ALS, helping raise $115 million for the ALS Association. The viral fundraiser nearly doubled the association’s annual research funding, expanding support to more than 500 research projects around the world.

Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine. Find out how much you could save in a year with a membership.
ALS is a progressive disease with no cure. It is also rare: About 30,000 people in the United States have it. Conditions that affect so few people seldom get that kind of public attention, or that kind of money. The Ice Bucket Challenge “brought a lot of attention to a rare disease and to the gaps that existed,” says Kuldip Dave, senior vice president of research at the ALS Association. “It brought focus to a disease that was, frankly, unknown.”
What is known about ALS? And has the Ice Bucket Challenge made a difference?
What is ALS?
You might know ALS as Lou Gehrig’s disease, named for the New York Yankees first baseman who retired after developing the disease in 1939 at age 36.
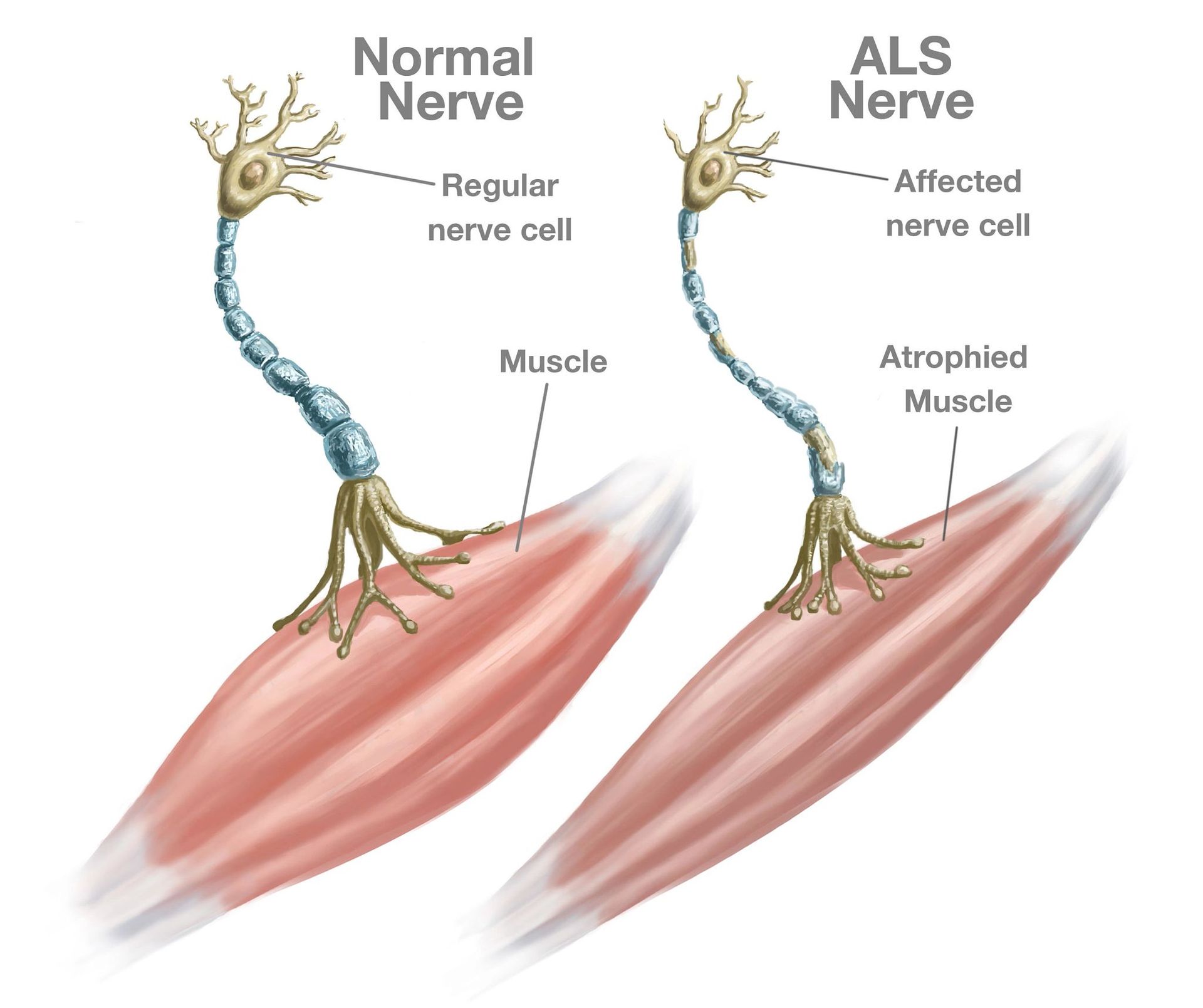
In ALS, nerve cells in the brain and spinal cord that control muscle movement and breathing deteriorate and die. Those cells, called motor neurons, can no longer send messages between the brain and the muscles, so the muscles weaken, start to twitch and waste away, or atrophy. Eventually, the brain cannot control voluntary muscle movements such as walking, talking, chewing and, eventually, breathing.
“These motor neurons start slowly dying. That’s why you slowly get weak. It doesn’t happen abruptly, like with an acute injury. But why these cells start dying? Honestly, we don’t fully understand,” says Jeffrey Rothstein, M.D., director of the Robert Packard Center for ALS Research at Johns Hopkins Medicine.
ALAMY STOCK PHOTO
What are the symptoms of ALS?
Weakness in an arm or leg, trouble swallowing or slurred speech are the most common first symptoms. The weakness may be preceded by twitching or cramps in the arms, shoulders, legs or even the tongue. But these aren’t the only possible early symptoms. The way ALS first shows up varies a lot from one person to another.
Symptoms of ALS
- Weakness, muscle atrophy, twitching or cramps in muscles of arms or legs
- Slurred speech, difficulty chewing or trouble swallowing
- Trouble walking or doing daily activities
- Tripping, falling or clumsy movements related to the hands or feet
- Laughing, crying or yawning at inappropriate times
“For some people, it might be only their arms that are weak for years before the legs get weak,” Rothstein says. In others, he says, muscles used for breathing, chewing and speaking are damaged early on, and the arms are affected very slowly.
ALS usually doesn’t affect the senses, including the ability to taste, smell, touch and hear. People with ALS usually remain able to reason, remember and understand, which means they are aware of the progressive loss of function. Less often, people with ALS experience changes in their behavior or the way they think or act. This happens to some degree in about half of people with ALS, according to the
most recent diagnostic criteria for the disease. These changes are often mild. About 8 to 9 percent of people who experience these cognitive changes will develop dementia and no longer be able to make decisions about their care.
Who gets ALS?
An estimated 5,000 people are newly diagnosed with ALS each year in the United States. Even though it’s not clear what causes ALS, certain people may be more likely to get it.
A small proportion of the people who get ALS — about 1 in 10 — were born with a gene mutation that caused the disease. Their children run a 50-50 chance of having this mutation, too. In most cases, just inheriting the gene from one parent is enough to ensure that a person will develop what’s called familial, or genetic, ALS.
About 25 to 40 percent of people with familial ALS have defects in a gene called C9orf72. Another 12 to 20 percent of familial cases have ALS due to a defect in a gene called SOD1. People who have C9orf72, the most common inherited gene mutation for ALS, may be at higher risk for a form of dementia called frontotemporal dementia (FTD). The same gene mutation in a family can cause ALS, FTD or both. “You can have a sister with ALS and a brother with FTD,” Rothstein says. “We don’t think of ALS as a dementia disease, but sometimes you can have a very severe dementia with it, which is usually because of that gene mutation.”
The vast majority of people with ALS — 9 in 10 — did not inherit a gene from a family member and have no family history of the disease. They have what’s called sporadic ALS. Age and, to a certain degree, sex are the only known risk factors for sporadic ALS. The age at which the disease is most often diagnosed is between the 50s and mid- 70s. Familial ALS may develop much earlier, around age 45 or younger.
Before age 65, ALS is a little more common in men than in women. After age 70, rates are the same for both sexes.
Aside from these known risk factors, smokers may be more likely to develop ALS, as are people who’ve been exposed to environmental toxins, such as lead or certain chemicals, research suggests. For some reason, perhaps due to toxic exposures, people who have served in the military seem to be at higher risk.
Is there treatment for ALS?
There’s no cure for ALS. People who have it will eventually die from the condition. Three medications approved by the U.S. Food and Drug Administration may slow the progression of the disease. Additional medications are used to treat symptoms and prevent complications to make patients comfortable and live as well as possible with ALS.
Kuldip Dave of the ALS Foundation recommends patients receive treatment at a multidisciplinary clinic “to interact with a team of health care professionals, not only a neurologist or ALS specialist, but also a physical therapist, pulmonologist, respiratory therapist and nurse coordinator.” Speech therapists, dietitians and social workers may also be part of the team. “Multiple publications show that people with ALS [who attend] a multidisciplinary clinic have at least a 10- to 18-month increased survival,” he says.
What can you expect with ALS?
ALS eventually weakens the muscles used for mobility, breathing, speaking and swallowing. You may need technology, devices and eventually professional care to help with each of these. For some people, ALS can progress to this point very quickly, and for others it can take years. Doctors typically won’t be able to let you know how fast the disease will progress.
No matter how quickly or slowly, ALS does progress over time. Eventually, people with this condition need more care than a spouse or adult child alone can provide. “Home caregivers are very common for ALS patients somewhere in the course of the disease, and, of course, at the very end, there can be hospice,” Rothstein says.
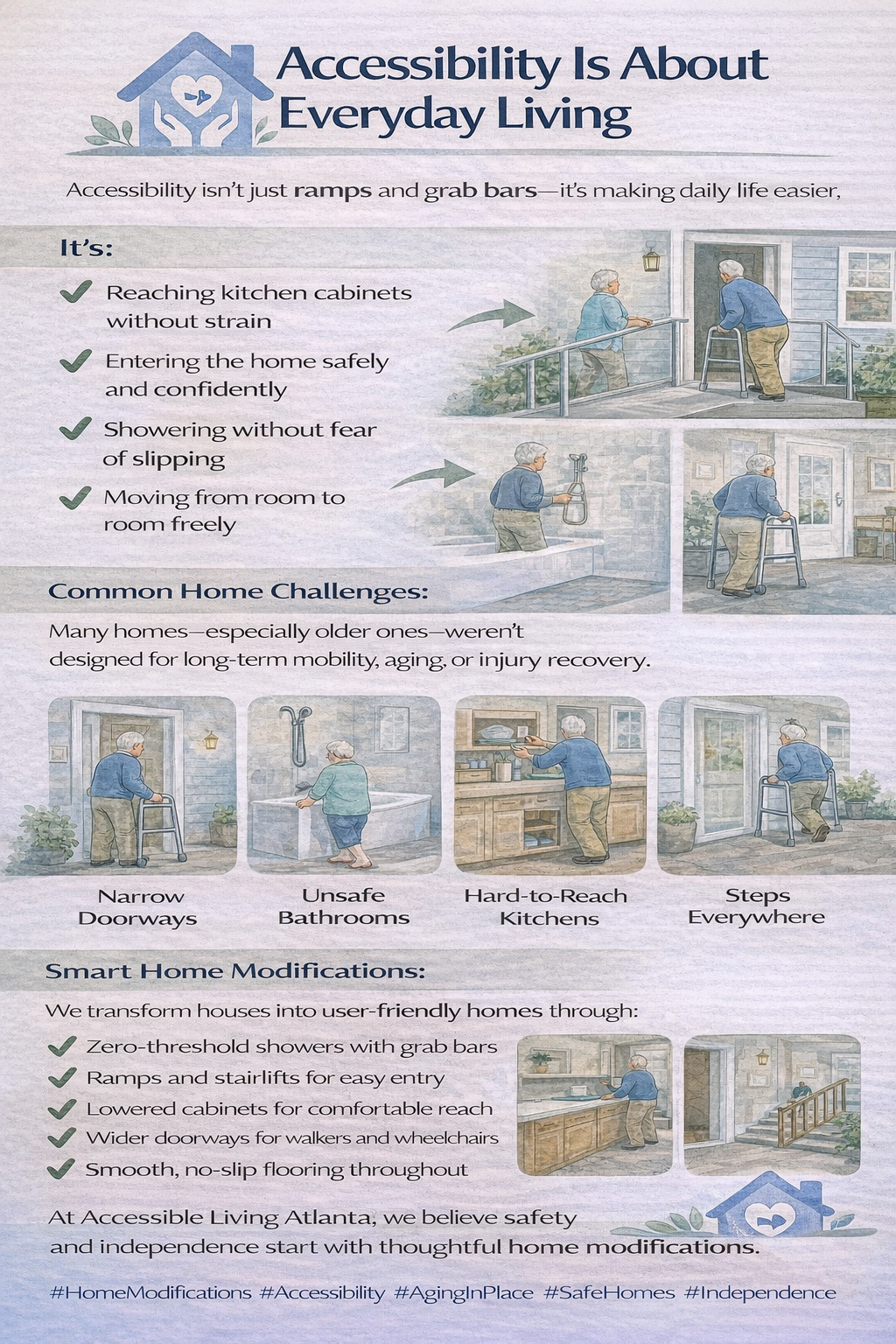
A variety of assistive devices are available to help people with ALS move around their homes, speak, breathe and carry out other tasks of daily living as the disease progresses. Assistive technology is also an area of active research in ALS to bring more effective tools to patients.
Though currently available drugs may slow the progress of ALS by a few months, they won’t cure it, halt it or reverse the damage. But scientific understanding of ALS — expanded in part by the Ice Bucket Challenge — has advanced in recent years.
For one, researchers have made some headway in treating familial ALS. There are around 40 known genes that cause genetic ALS. In 2023, the Food and Drug Administration approved Qalsody (tofersen), the first drug to target one of those genes, SOD1, believed to be mutated in 1 to 2 percent of people with ALS.
In a clinical trial, when people with ALS due to SOD1 mutations received Qalsody intraspinal injections (three loading doses every two weeks followed by five monthly maintenance doses), levels of a protein called neurofilament-light (NfL) that is elevated in people with ALS began to drop. The drug received accelerated approval because of the need for effective therapies, and the reduction in NfL is considered a predictor of patient benefit. Researchers will continue to study the drug to see if it actually has an effect on the progress and symptoms of the disease.
Medications for ALS
Available treatments for ALS do not reverse damage or provide a cure. They may slow disease progression, extend survival and improve quality of life.
- Qalsody (tofersen): given by spinal injection in the 1 to 2 percent of ALS patients with a mutation in the SOD1 gene. It may decrease neuron damage.
- Radicava (edaravone): an antioxidant given orally or intravenously that may slow functional decline.
- Rilutek (riluzole): an oral medication that may reduce damage to motor neurons by reducing levels of glutamate, a chemical messenger between nerve cells. In clinical trials, riluzole prolonged survival in people with ALS by a few months. It’s available in thickened liquid form (Tiglutik) or as a tablet that melts on the tongue (Exservan).
- Nuedexta: an oral medication that treats involuntary outbursts of crying or laughing in people with ALS and other neurological disorders.
AARP's Brain Health Resource Center
Find more on brain health plus dementia, stroke, falls, depression/anxiety and Parkinson's disease.
“The important thing is that they were able to develop a therapy that went straight for that gene and repaired it,” Dave says. He’s optimistic that the same approach can be used to mute the effects of other genes gone awry in ALS: “Now we have the formula to do this for the other 39 genes.”
NfL is the focus of other ALS research, beyond those people with familial ALS. Researchers are getting closer to understanding how to use this protein as a blood biomarker for the disease in all patients. This could lead to earlier detection and, potentially, drugs that target the protein directly as a way to stop the disease.
The last 10 years of extra support for ALS research have led to a larger-than-ever diversity of research. More than 35 clinical trials are recruiting U.S. patients affected with ALS to test new therapies. Promising work is underway in the following areas:
- Repurposing anti-inflammatory drugs. It’s known that inflammation underpins neurodegenerative diseases, including ALS. A growing number of drug companies are taking an interest in ALS and testing the impact of existing anti-inflammatory drugs for people with ALS.
- Correcting defects in TDP-43. This protein in the nuclei of cells in the central nervous system plays a crucial role in their function. But in ALS, a specific defect puts TDP-43 outside the nucleus of motor neurons. Researchers are testing a drug that moves the protein back in place, and they are now in the early days of developing ALS treatments based on this concept.
- Using brain-computer interfaces (BCI). An implantable device in the brain would allow people with ALS to use their thoughts to control computers, equipment and devices such as wheelchairs and breathing and speech assistance.
“For a rare disease like ALS, having that many opportunities is a good thing,” Dave says. “We don’t know where our next home run is going to come from. The fact that we have multiple ways to go after this disease is really exciting.”
#homeaccessibility #homemodification #homehealthcare #aginginplace #aginggracefully #caregivers #disability #disabilityawareness #wheelchairuser #wheelchairaccessible #spinalcordinjury #physicallychallenged #safetyathome #elderlycare #graytsunami #healthylifestyle #accessiblematters #userfriendlyhome